Description
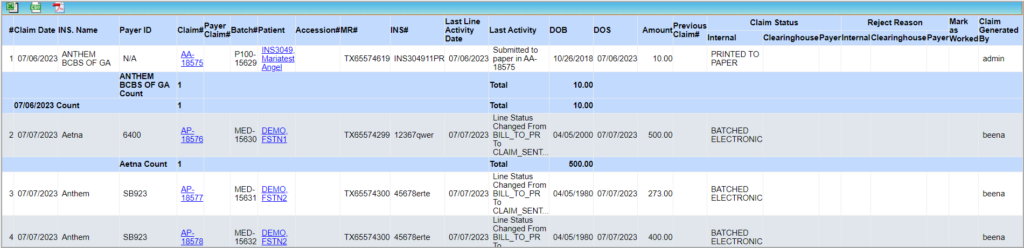
The report shows the list of claims batched electronically or on paper for the selected date period. For the paper claims, the printed status is indicated on the report, and for the electronically submitted claims, the clearinghouse and payer response status with the response details are shown on the report.
Significance
1. This is very similar to the G4 report. The major difference is that the G1 report displays remarks and reject reasons from payers, clearinghouses, etc., whereas the G4 report shows procedure codes and line status.
2. The G1 report has an offline reporting feature.
Utility
1. If you want to view only the electronic claims or only the paper claims, use the ‘Claim batch type’ filter.
2. Service location and encounter-level provider information are available in the Excel output.
3. The last column, ‘Claim Generated By‘ will show the user who generated the claim.
Search filters for the G1 report
| Field | Description |
| Claim Date | Provide the claim date range |
| DOS | Provide the DOS range |
| Patient | To filter by a specific patient |
| Legal Entity | To filter results pertaining to a specific legal entity |
| Provider | To filter results for a specific provider |
| Insurance/Payer ID | To filter by insurance |
| Insurance Level | To filter by Insurance level |
| Claim Batch Type | Paper, EDI |
| Clearinghouse Status | To view claims having a specific CH status |
| Interchange# | Unique number of the batch |
| Claims Receiver | To view claims sent to a specific CH |
| Payer Status | To filter results for a specific payer status |
| Claim# | To view report for a single claim |
| Include COB claims | To include Cross over claims in the result |
| Sort | Select Claim#, Insurance or patient Last name to sort the result |
Search screen of G1 report
Sample G1 report
Possible Outputs of G1 Report
![]() Excel output Fields in the Excel output of G1 Report
Excel output Fields in the Excel output of G1 Report
![]() CSV output Fields in CSV file of G1 Report
CSV output Fields in CSV file of G1 Report