PracticeSuite Release Note
Product Release Version: 19.6.5
EHR Version: EHR-18.0.0
Product Release Date: September 2020
© 2020 PracticeSuite
Disclaimer: All rights are reserved. No part of this work may be reproduced in any form or by any means through graphic, electronic, or mechanical, including photocopy, recording, or information storage and retrieval systems – without written permission of the publisher.
The products that are referred to in this document may be either trademarks and/or registered trademarks of the respective owners. The publisher and the author make no claim to these trademarks.
While every precaution has been taken in the preparation of this document, the publisher and the author assume no responsibility for errors or omissions, or for damages resulting from the use of information contained in this document or from the use of programs and source code that may accompany it. In no event shall the publisher and the author be liable for any loss of profit or any other commercial damage caused or alleged to have been caused directly or indirectly by this document.
Printed September 2020 at 37600 Central Court, Suite# 260, Newark, CA 94560
Part – 1 Enhancements
1.1 EHR Advanced- Patient Details to be Shown in Clinical Quality Measures(CQM)
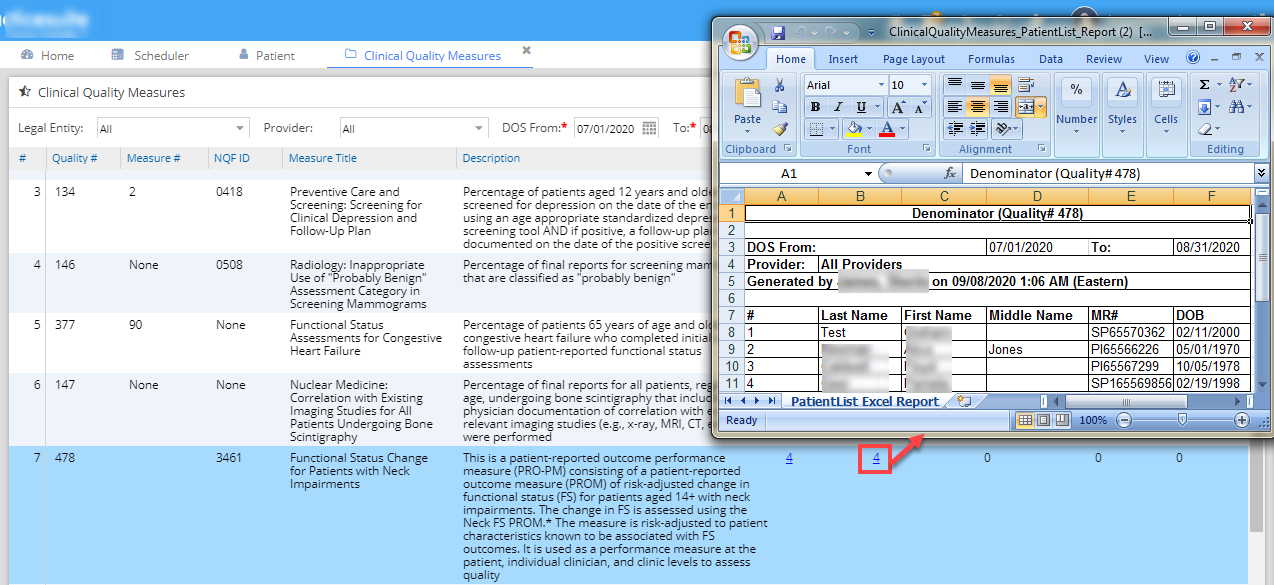
For each Clinical Quality Measure, the patients queried for the reporting measure can be listed from the CQM screen. The columns ‘Initial Population’ and ‘Denominator(Eligible Instances)’ are made hyperlinks, when clicked on the link, it opens an excel spreadsheet listing the patients used in the measure calculation. Image 1.1 demonstrates this.
1.2 ERA Posting
1.2.1 ERAs with CO-144 negative adjustments can hereafter be auto-posted.
1.2.2 Secondary claim rejections due to missing/mismatch in primary adjustment breakup issue has been resolved.
1.3 UB04 Charge Entry – New Rev Code
A new Revenue Code- “1003” (description – “TRANSITIONAL/SUPERVISED CARE R&B BH”) added to the UB-04 Rev. Code repository in PracticeSuite.
1.4 Patient Statements
1.4.1 When using the filter ‘No Payment Received since’, all auto adjustment payment entries and ‘0’ dollar payments would going forward be excluded for querying the statements list.
1.4.2 Added a new field named- “Patient A/R Date” to Patient Statement CSV. This is the activity date and is the date when the charge line was changed to patient responsibility line status (such as – Bill_To_PT/GR).
1.5 EHR- Prescription Review by Supervising Provider
Prescriptions ordered by a mid level provider can now be reviewed seamlessly by the supervising physician. Previously, there were some difficulties for the supervising providers to review their assisting Provider’s Rx.
1.6 KPI Dashboard Update
A few changes are made in the calculation of some of the performance indicators and revenue cycle parameters. The parameters along with the changes are listed below.
a. Net Collection Rate– Calculation to be driven by Accounting Date instead of Claim date. Only insurance adjustments are now included in the calculation and the 90 day look back has been dropped from the report.
b. Gross Collection Rate– Calculation to be driven by Accounting Date instead of Claim date. The 90 day look back has been dropped from the report.
c. Total Charge– An aberration in the calculation of this KPI has been resolved. The numbers in the report will now match the other charge/ar reports such as D10 or J9.
d. Change in A/R– An aberration in the calculation of this KPI has been resolved. The numbers in the report will now match the other charge/ar reports such as D10 or J9.
e. Days in A/R– An aberration in the calculation of this KPI has been resolved.
f. Percent of A/R over 120 days– Insurance, Percent of A/R over 120 days-Patient
For both the revenue cycle parameters, year-to date numbers are also now included in the report. For Patient A/R, lines in “In Collection” status are excluded from the A/R calculation.
1.7 Payment
1.7.1 Payer ID in Payment Entry and Posting Screens
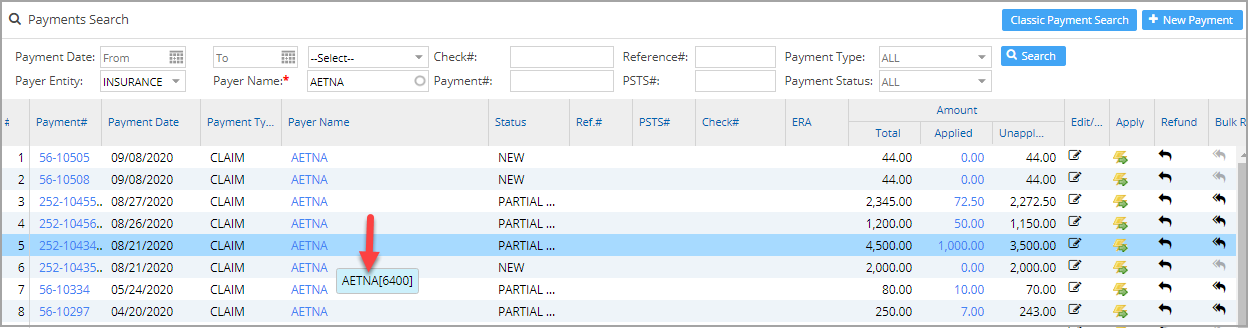
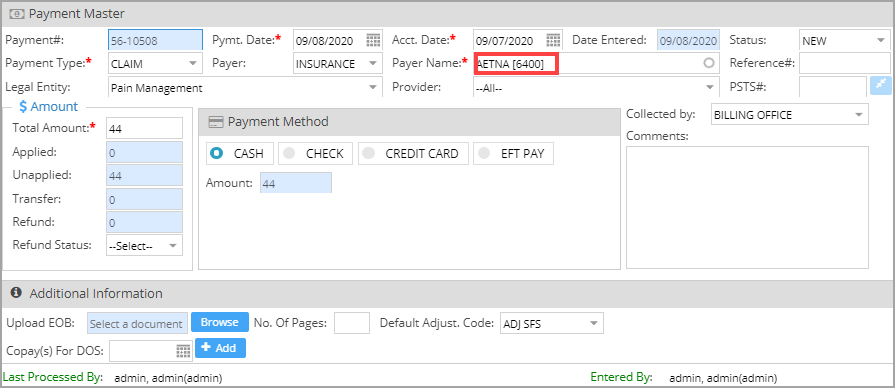
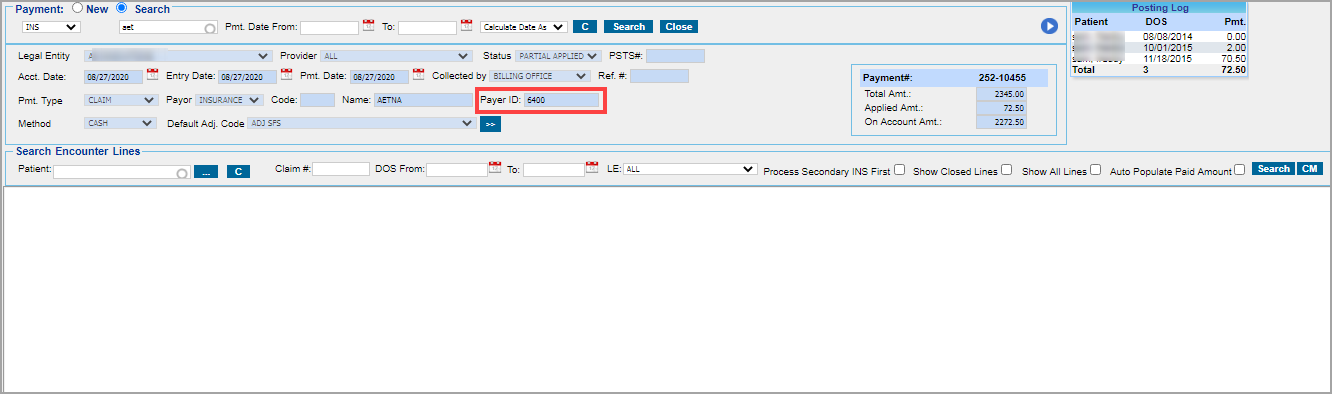
Payer ID# of the insurance selected in the payment entry will henceforth be displayed in both the Payment Entry and Payment Posting screens. In the Payment Search screen it can viewed on mouse-over of payer name. On the Payment Posting screen, the payer id will be visible in the “Payer ID” field next to the payer name. Please see screenshots- Image 1.7.1a, Image 1.7.1b, and Image 1.7.1c.
1.7.2 Payment Posting – On Account Balance
An ‘On Account’ field has been added to the existing line of subtotal fields at the bottom of the Payment Posting screen. This helps users to see on the fly the on account balance even before it is applied to the lines.
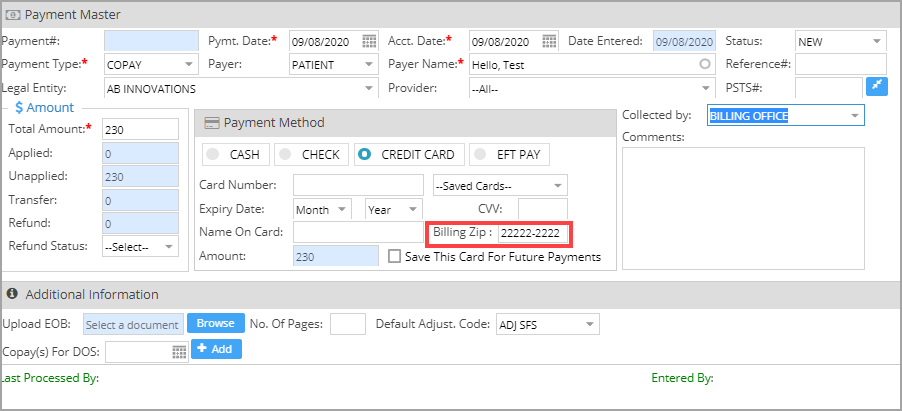
1.7.3 Credit Card Payment – Billing Zip Code Field
As certain banks have mandated the use of zip codes for the credit card processing, USIO payment gateway integrated accounts will need to enter the billing zip code to complete the transaction. A user editable zip code field has been added in the entry screen. If the billing zip code is left blank on entry, the patient’s zip code will be used for the transaction. Practice’s zip code will be populated as the billing zip code if both the card holder’s zip code (payment screen) and the patient’s zip code (in demographics screen) are blank. Image 1.7.3 shows the new field in Payment Entry Screen.
1.7.4 Clearing of Payer Name on Changing Type
In the Payment Entry screen, the Payer Name will no longer be cleared when the selected Payment Type of the payment is changed to any of the other Patient Payment Types. However, changing the Payer Entity on the payment will clear the selected payment type.
1.8 CMS/HCFA Form
Changed to a darker font style for better print visibility and readability.
1.9 Collection Manager- Flexible Drag for Search Filters & Claims Listing Section
Users can now adjust the grid size for both the search section & the claims listing section within Collection Manager screen. Previously, the flexible drag feature was limited to the category listing section. Play the below video to see how to make the grid adjustments.
Part 2. Reports
2.1 New Patients Report
This existing report has been updated to list both new and established patients driven by procedure code and not plainly based on patient creation in the system. See Image 2.1.
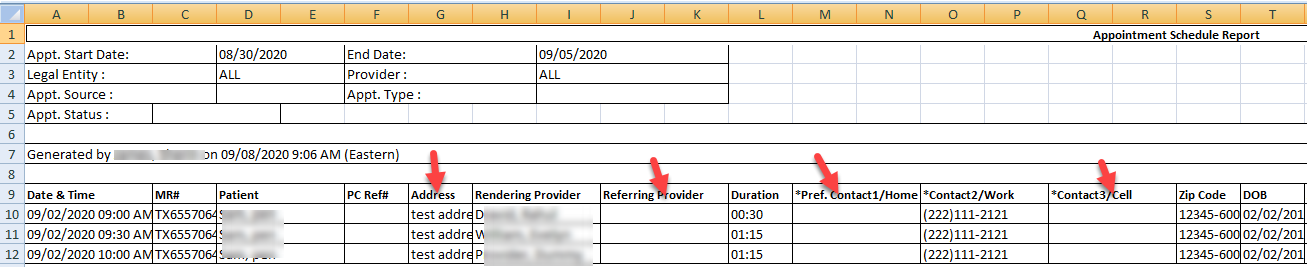
2.2 New Fields in A1. Appointment Schedule Report
Patient Address, Phone number and Referring Provider information fields added to the A1 report excel format. In addition, the ‘Appointment Created By’ info is added to the excel. Please see Image 2.2.
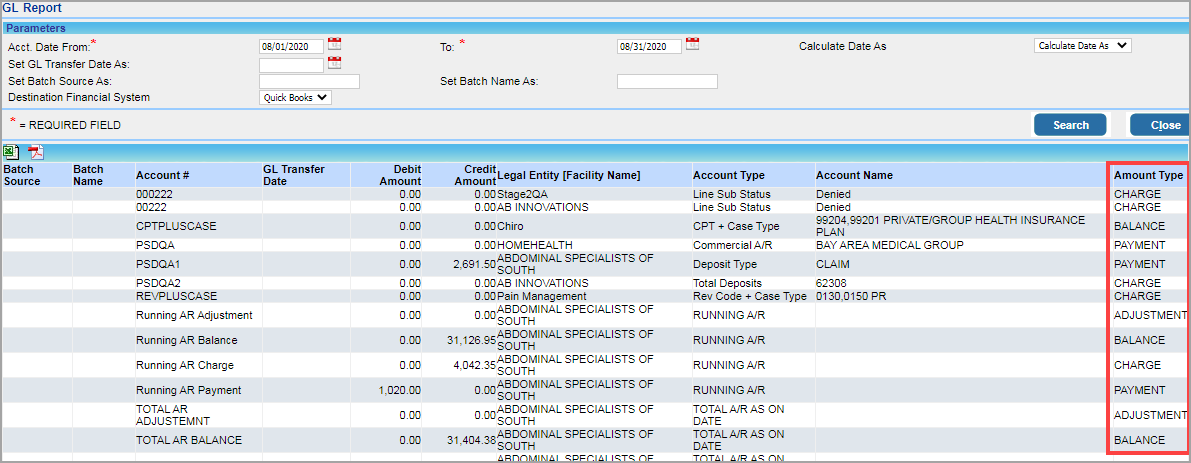
2.3 New Field Amount Type in GL Report & GL Detailed Report
A new field ‘Amount Type’ added to both GL report and GL Detailed Report. This helps in identifying the type of transaction and whether the amount type is for – charges, payment, adjustment or balance. Image 2.3 shows the Amount Type fields within the red marker.
2.4 New Field – On Account in D3. Summary- Patient/Guarantor Balance and Aging Report
A new field named ‘On Account’ added to the D3 report. This shows the patient’s on account (unapplied/credit balance).
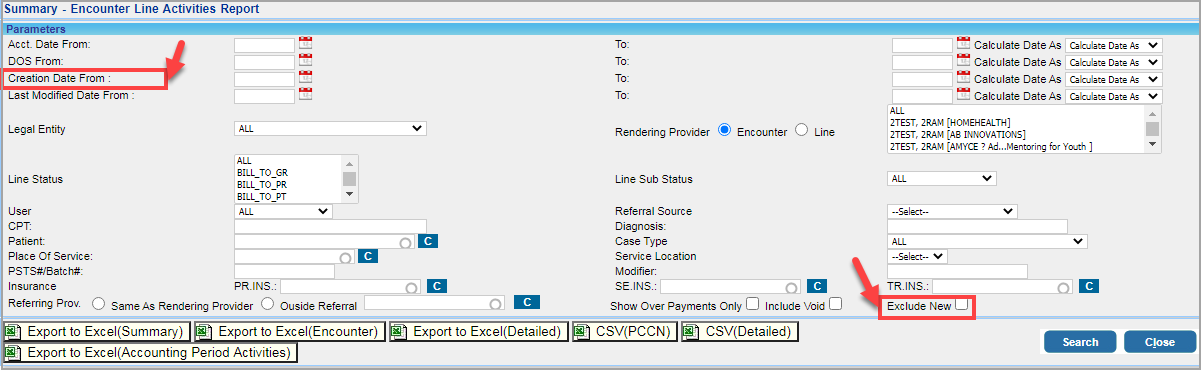
2.5 New Report Filters – I8. Summary Encounter Line Activity Report
2.5.1 A new report filter Creation Date added to the search parameters section in I8 report. Users can filter the report for a single charge creation date or creation date range. Additionally, another report filter checkbox named ‘Exclude New’ has also been added to the report filters. When the report is run with the box checked, all unposted charges are excluded from the report data. Please see Image 2.5.1 shows the new added filters.
2.5.2 Performance Improvement – I8. Summary Encounter Line Activity Report
Performance improvements have been made to both the excel and CSV outputs of the I8 report.
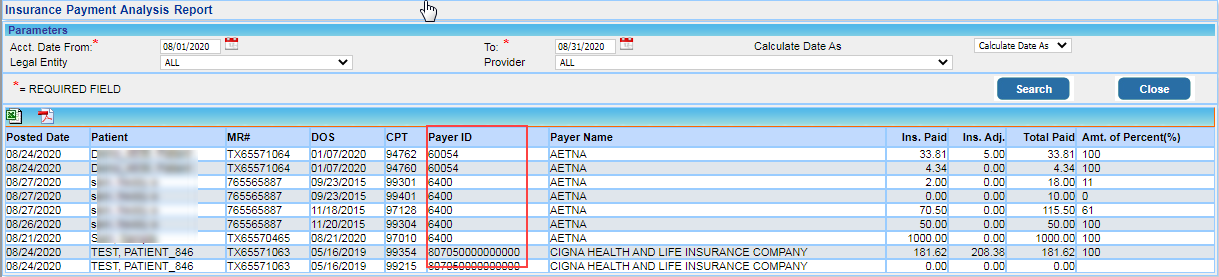
2.6 New Field – I19. Insurance Payment Analysis Report
‘Payer ID’ field added in I19 report. Please refer Image 2.6.
Part 3. Bugs
3.1 ERA
3.1.1 CoB Payer Auto-creation: Patient to Payer Mismatch
If ERA based automation for secondary payer creation is turned on (from Billing Options) in the account, when the secondary cob payers were being auto created, the patients were getting mapped to the wrong payers. This patient to payer mapping error has now been addressed.
3.1.2 Error in ERA Search Filter
In the ERA screen, ERAs can now be listed with the date parameters. Previously, the results would not have been displayed when running the search with the date filter.
3.2 Reporting Error in I9. Detailed- Encounter Line Activities Report
When running I9. Detailed Summary Encounter Line Activities Report with the date of service parameter, there were discrepancies in the paid and adjustment amounts populated in the report. This error has been addressed and the numbers will now match with other payment reports such as Posting Details Report.
3.3 EMR Level 2 Duplication Issue
Level 2 items were being duplicated in some instances. This issue has been resolved.
3.4 Training Videos
In-app training videos were not opening in full screen mode. This issue has been addressed.
3.5 HTML Tags Visible in Patient Notification Report
When the report is opened by selecting a patient, HTML codes used to be visible in the report. This issue has been resolved.