PracticeSuite Release Note
Product Release Version: 19.8.7
EHR Version: EHR-18.0.0
Product Release Date: June 2021
© 2021 PracticeSuite
Disclaimer: All rights are reserved. No part of this work may be reproduced in any form or by any means through graphic, electronic, or mechanical, including photocopy, recording, or information storage and retrieval systems – without written permission of the publisher.
The products that are referred to in this document may be either trademarks and/or registered trademarks of the respective owners. The publisher and the author make no claim to these trademarks.
While every precaution has been taken in the preparation of this document, the publisher and the author assume no responsibility for errors or omissions, or for damages resulting from the use of the information contained in this document or from the use of programs and source code that may accompany it. In no event shall the publisher and the author be liable for any loss of profit or any other commercial damage caused or alleged to have been caused directly or indirectly by this document.
Printed June 2021 at PracticeSuite, Inc.3206 Cove Bend Dr Suite A Tampa FL 33613
Part – 1 Enhancements
1.1 Patient Demographics
1.1.1. Case Switch
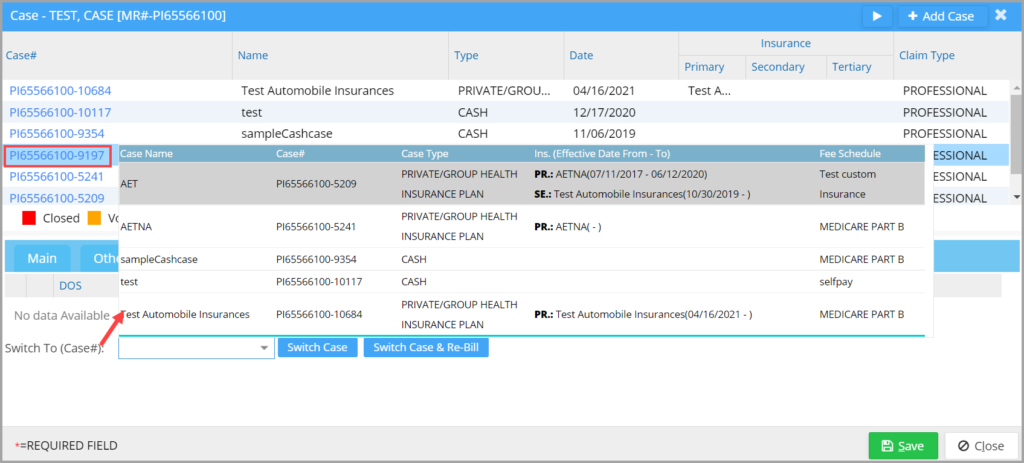
A. Case Dropdown – Case Switch Screen
In the Case Switch screen, additional fields are now shown in the dropdown. New fields made visible on the screen are- Case Type, Fee Schedule, Primary, Secondary, Tertiary insurance names, and effective dates in addition to the Case Number and Case Name.
B. Case Switch for Paid Encounters
Hereafter, system will allow even paid encounters to be switched if the insurance/policy # and insurance level in the original Case match that of the target Case. Previously, an encounter could only be switched to the other case if no insurance payment was applied for that encounter.
Additionally, if switching an encounter from insurance to cash case, all lines in the encounter will be changed to BILL_TO_PT status.
1.1.2 Procedure Code Count Tracking for Authorizations
If procedure codes are added in the authorization, the system will track the used procedure count.
1.2 ERA
1.2.1. Select Claim(s) Option in ERA Posting Screen
In the ERA Posting screen, a new option is introduced for users to select the claims for posting. With the new update, users can partially post an ERA and then return later to complete the rest. This is particularly helpful when posting large ERAs.
A checkbox has been added next to each claim in the ERA Posting screen and users can choose to either post them all or to partially post the ERA; see Image 1.2.1. To ease the claim selection for users, any line(s) touched by the user will be autoselected for posting.
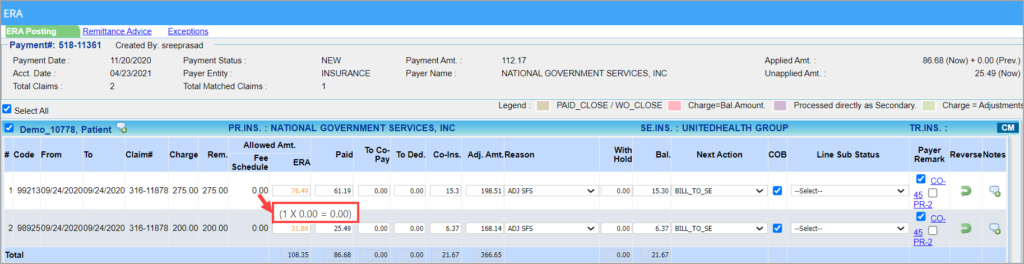
1.2.2. ERA Posting- Allowed Amt Changes
1. The following headers have been renamed in the ERA Posting screen:
a. “Fee Sch. Allow.” changed to “Allowed Amt. (Fee Schedule)“.
b. “Allowed Amt” changed to “Allowed Amt. (ERA)”.
2. Mouseover on ‘Allowed Amt (Fee Schedule)’ will display per unit allowed and the calculated allowed amt based on the no. of units; see Image 1.2.2.
3. ERA Allowed Amount to be red-texted on the ERA Posting screen if less than the calculated allowed amount based on the fee schedule and orange-texted if it is higher.
4. Color coding introduced in ERA Posting screen has also been rolled out to the Manual Payment Posting screen.
1.3 Charge Master
1.3.1 Resubmission Code and Original Ref. # to be Shown in Encounter Activity
A. Any change made to the Resubmission Code and Original Ref# fields will be recorded as an encounter activity in Charge Master.
B. A new validation is added for the ‘Original Ref. #’ field. If the dropdown option selected in the Resubmission Code field is either “Replacement of Prior Claim” or “Void or Cancel of Prior Claim”, the Original Ref # entry has been made mandatory.
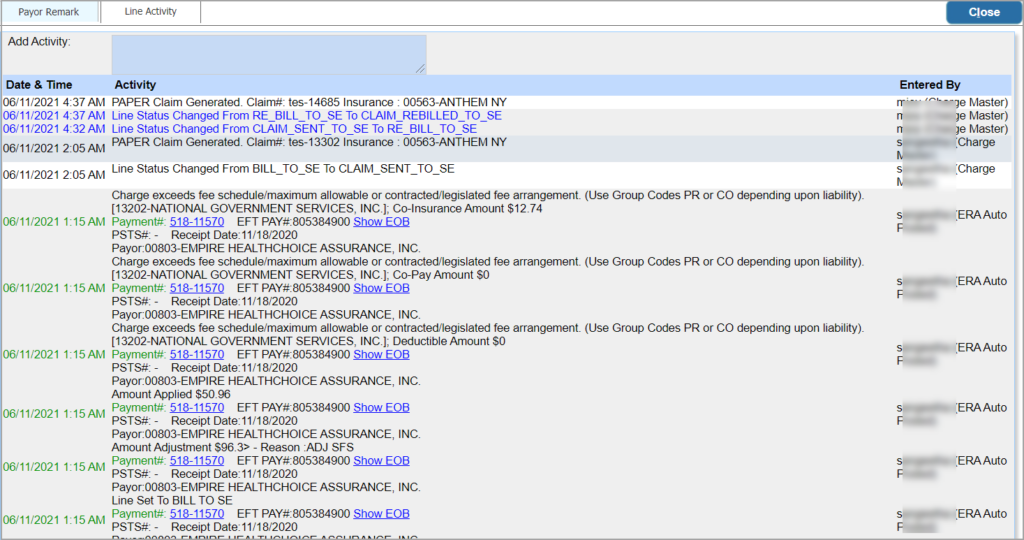
1.3.2 Line Activity Color
Date & Time and Activity in the Line Activity screen will be color-coded as in Image 1.3.2. A change from the previous is that only the text will be colored and not the background.
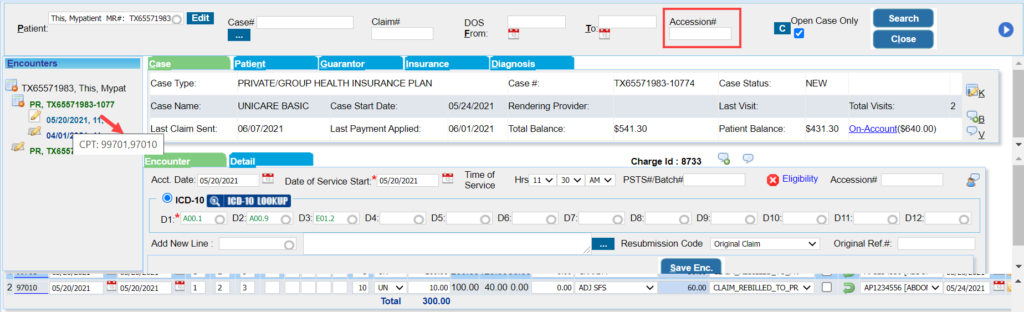
1.3.3 Accession# Search and Procedure Code Tooltip in Charge Master
a. Accession # search filter added in Charge Master screen to search by the superbill # generated from the partner/ external system. Please see Image 1.3.3.
b. Mouseover on the left-hand side date of service listing will show the procedurencode(s) present in the encounter. See Image 1.3.3.
1.4 Voided Refunds
For any voided refunds, users can now view the refund activity in the parent payment entry screen.
1.5 XSuperbill- Accession# and Last Modified User Search
A. ‘Accession#’ and ‘Last Modified User’ search filters added in X-Superbill screen.
B. BILL_TO_PT lines can be changed to BILL_TO_GR and vice-versa from the X-SB screen.
C. Provider titles for rendering and line-level providers are now displayed on the X-SB screen.
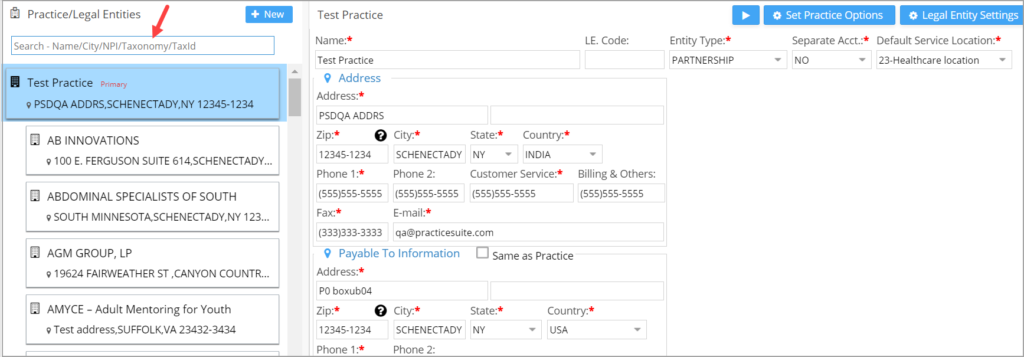
1.6 Legal Entity Search
A Legal Entity search filter is added on the Legal Entity listing pane. Users can use this single filter to search LEs by any of the following parameters- Name, City, NPI, Taxonomy or Tax Id (refer Image 1.6).
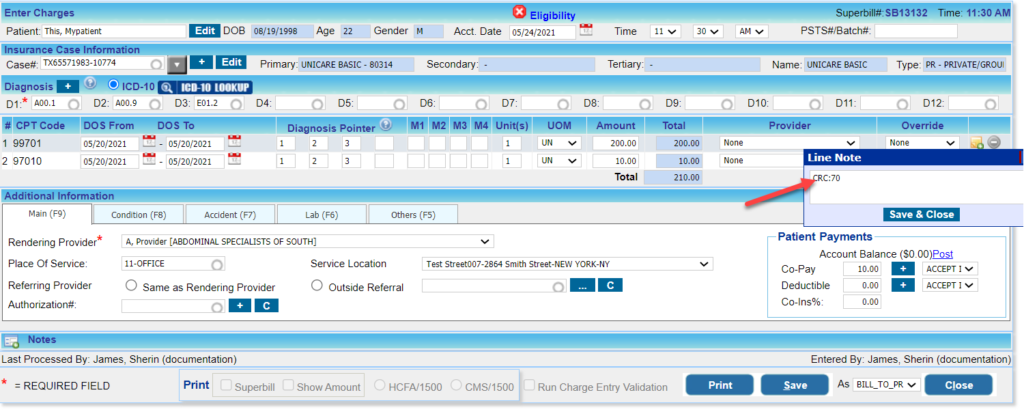
1.7 EDI
1.7.1 Hospice Employee Indicator
In loop 2400 of the electronic claim that references the Hospice Employee Indicator, CRC segment is mandatory for all Medicare claims involving physician services for hospice patients. This info can be included by entering “CRC:70” in the line note; see Image 1.7.1
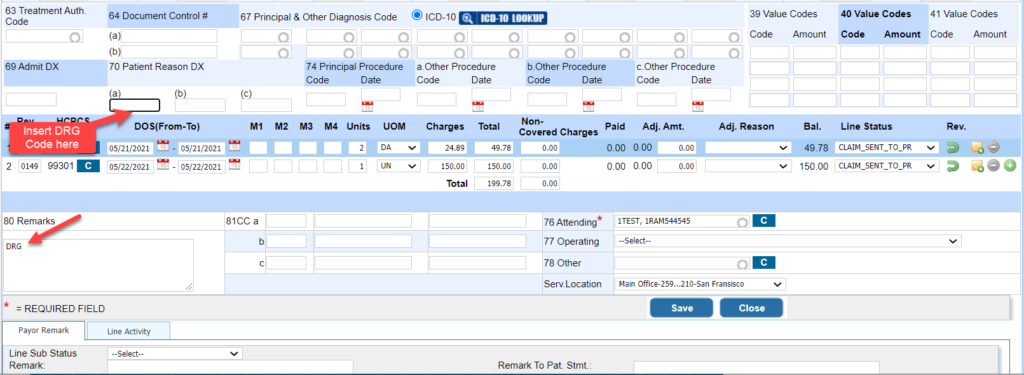
1.7.2 DRG Code in Institutional Claims
The DRG info can be included in the claim by entering the DRG code in box 70(a) and the exact text “DRG” in box 80; see Image 1.7.2
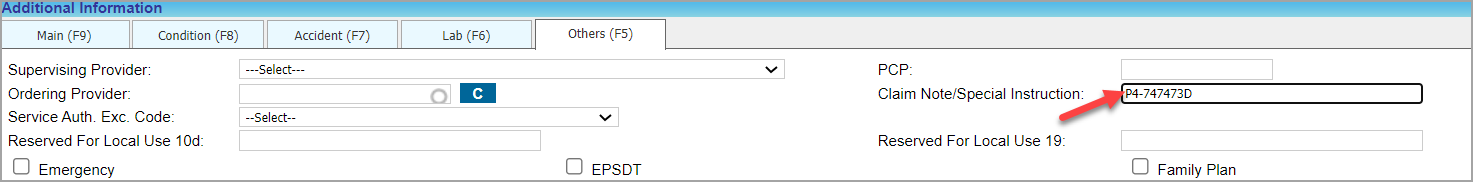
1.7.3 Demonstration Project Identifier
To populate “Demonstration Project Identifier” in electronic claims under 2300>Ref segment with qualifier ‘P4’, in the Claim Note enter “P4” followed by a dash (hyphen) and then the DPI. Such as, “P4-1234567D” where ‘1234567D’ is the DPI; refer Image 1.7.3.
1.8 Fee Schedule Amt Population for Procedure Code-Modifier Combination
For charges received through the interface, previously it was required to have the same Procedure code-Modifier combination in the fee schedule for the amount to be populated.
With the new update, if the exact procedure and modifier combination is not found in the fee schedule, the system will match the closest combination to auto-populate the amount. If no modifier combination exists in the fee schedule for the particular procedure code, the system matches the procedure code to populate the amount.
1.9 UB04- Service Location Defaulted from Billing Options Setup
In UB04, the place of service and service location saved in Billing Options defaults as the service location when entering a new charge.
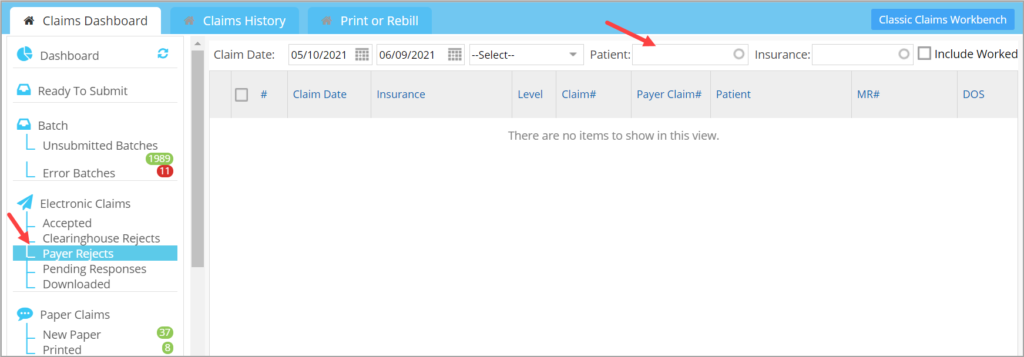
1.10 Claims Workbench- New Patient Filter
Patient Filter added for all response buckets. Image 1.10 shows the patient filter in the Payer Reject bucket.
1.11 New Manufacturer Added to Vaccine Manufacturer Repository
New manufacturer info:
Name: Moderna US, Inc.
MVX_CODE : MOD.
1.12 New ICD Code Added to our Repository
A new ICD 10 code U07.7; description “Covid-19 Vaccine (causing adverse effects in therapeutic use)” added to ICD-10 repository.
1.13 Statement# Tag for eStatements
E-Statement emails can now show the statement #. A new tag ” #@STATEMENT_NUM#@” has been made available for this purpose.
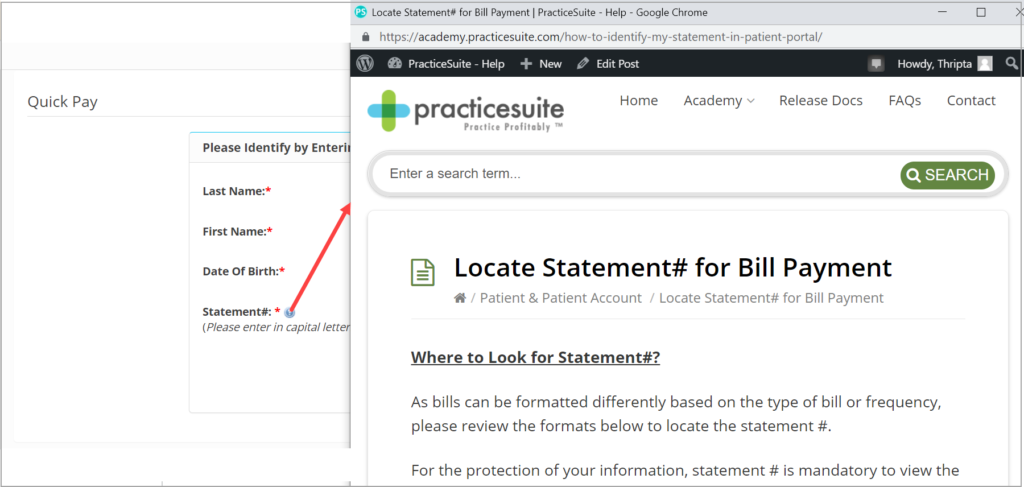
1.14 Patient Portal- Help Description For Statement # Field
When making an online payment, to help patients locate the statement # on their bill, a help icon has been placed next to the statement #. On clicking the icon, patients are directed to PracticeSuite’s academy page to view the article with screenshots that explains where they can locate the statement #. Please see Image 1.14.
1.15 Appointment Reminders- New Technology-Based Engine
Upgraded the appointment reminder engine. Also, hereafter a reminder will never be triggered by the system if it is past the scheduled appointment time.
Part 2- Reports
2.1 ‘B6. Appointments- Charges Reconciliation Report’
A new excel output is added to the report to show payment details in addition to the appointment and superbill status. Following are the fields that are added to the new excel output:
APPT DATE, PATIENT LAST NAME, PATIENT FIRST NAME, MRN, APPT STATUS, APPT REASON, LE, PROVIDER CODE, PROVIDER NAME, INS CO NAME, COPAY/DED/COINS AMT, HOW COPAY/DED/COINS PAID, DATE OF COPAY/DED/COINS, PAYMENT RECEIVED DATE, BILLED AMT, CPT CODES, FIRST DATE CLAIM BILLED, INSURANCE PAID AMOUNT, PATIENT PAID AMOUNT, DATE INSURANCE/PATIENT PAID, DATE INSURANCE PMT PROCESSED.
2.2 ‘I6. Posting Detail Report’- Insurance Info Added to Excel output
I6 report to include primary, secondary and tertiary insurances of the encounter in both the summary and detailed Excel outputs.
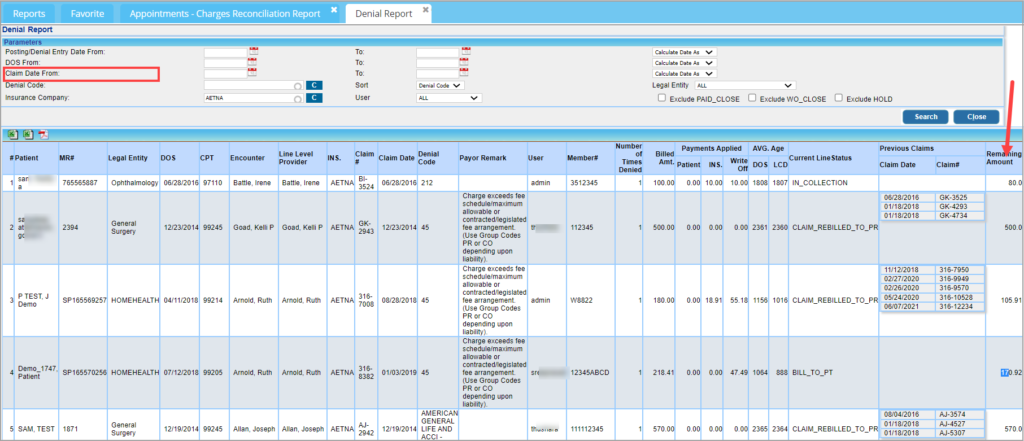
2.3 ‘G2. Denial Report’
2.3.1 Remaining Amount
The line balance info added to the report and will show under the field header ‘Remaining Amount’. Please see Image 2.3.
2.3.2 Claim Date Search and Additional Fields in Excel Report
Claim Date filter added to the report (see Image 2.3). Additional fields added to the excel output. The new fields in the report are- encounter-level provider, line-level provider, units, and modifiers.
2.4 ‘I8. Summary-Encounter Line Activities Report’ – Patient Creation Date Added
Patient Creation Date added to detailed CSV output and offline report of the I8 report.
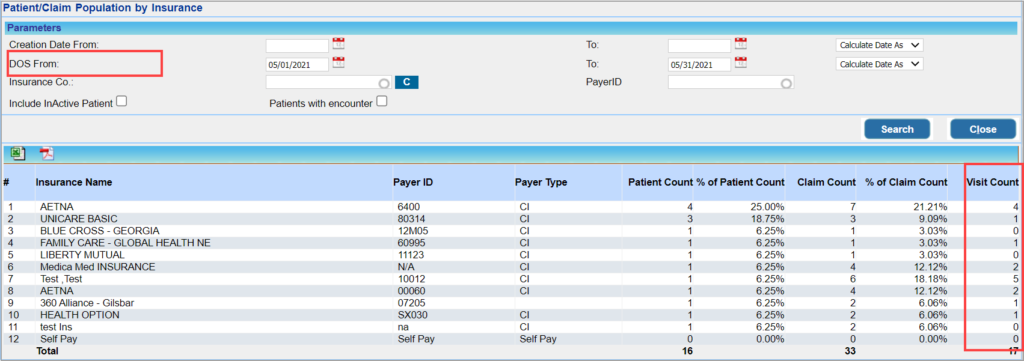
2.5 E8 Report now has DOS as Search Parameter and Visit Count in the Search Result
Users can now search ‘E8. Patient/Claim Population By Insurance Report’ with DOS (date of service) as the search parameter. The report now displays the visit count of patients under each insurance. Image 2.5 highlights the newly added DOS search field and the Visit Count column.
Part-3 Bug Fixes
3.1 Performance Improvement for J9. Daily /Month End Close Report
Fine-tuning of all queries in J9. Daily/ Month End Close Report is completed for faster report load.
3.2 Claim Status Response Issue
Claims rejected by the payer where multiple statuses are present in the 277 files were not showing up in the payer reject bucket. This has been addressed.
3.3 TeleMed: Resolved Documents Upload Issue
Resolved the issue where users were unable to upload documents on the telemed session.
3.4 Report Generation Fails- ‘J30. Key Summary Metrics’ Report
Legal Entity filter when selected as ‘ ALL’ failed to generate the J30 report. This issue has been addressed.
3.5 Clinical Desktop
3.5.1 Patient Demographic Info in CCR/CCD
For Patients registered through the patient portal, info such as Ethnicity, Language, and Race were not being presented accurately in the CCR section of EMR. The issue has been corrected.
3.5.2 Insurance Name in Chart
The plan name of the insurance used to be displayed on EMR screen and not the actual insurance name. This has been corrected to display the insurance name in EMR.
3.5.3 Screen Zoom Issue
Resolved the issue with the left and right side tabs not being visible on the Clinical Desktop when decreasing the screen zoom to 90 percent.
3.6 UB04: ‘Copy Last Superbill’
When using the ‘Copy last Superbill’ option in UB04 screen, the From and To Dates of the Statement Covers Period was being populated from the previous charge. This is now resolved.
3.7 Unposted Lines in J25 Report
On entering payment # for running the report, unposted lines were not being shown in the report result. This issue has been addressed.
3.8 ‘Fav KPI- Claims 45 days Away From Untimely Filing Limit’
Claims that are in ‘Claim_Sent_To_Pr’ status were erroneously shown in the Untimely Filing Limit category of the Favorite KPI. This is now fixed and only the claims in New and Bill_To_PR status will be included in the Untimely Filing Limit KPI.
3.9 Password Reset Functionality for SSO Group Login
Resolved the password reset issue for SSO users.
3.10 D15. and J9 Reports Mismatch Resolved
A mismatch between D15. Aging Report as of Accounting Date and J9. Daily/Month End Close Report is now corrected.
3.11 Payment Number Display Corrected in I14 Report Excel
Resolved the payment # formatting issue in the excel output of ‘I14 Payment Activity Report’.