Claim History
Claim history gives a view of all submitted claims. Claims are sorted in reverse chronological order, with the most recent claim date appearing first.
Search Filters of Claims History
Search Filters
Claim Date, Insurance, Claim #, DOS, Patient, Claims Receiver, Insurance Level, Legal Entity, Provider, Payer Claim #, Claim Batch Type, Interchange #, Clearinghouse Status, Payer Status, Line Status, Line Sub-Status.
Sort Options
Claim Date, Claim#, Insurance, Patient Last Name.
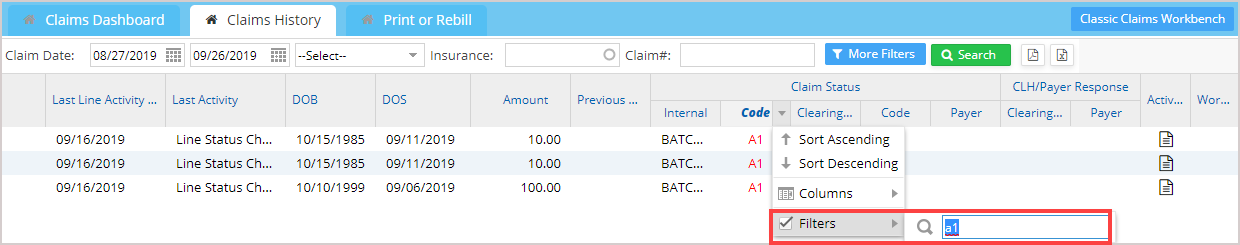
Column Filters
All columns except date, amounts, and number fields have filters to narrow down the search results. The filter applied for the status code with value a1 is illustrated in Image 3.
Output Options
Important Columns in the Claims History screen
| Column | Description |
| Claim Date | The date on which the claim was generated |
| Insurance | Name of the Insurance |
| Level | P-Primary S-Secondary T-Tertiary |
| Claim# | System-generated unique number for the claim |
| Payer Claim# | |
| Batch# | The unique number of the batch in which the claim was sent |
| Patient | Name of the patient in the claim |
| Accession# | Accession# number of the patient |
| MR# | MR# of the patient |
| INS# | Member ID provided by the insurance for the subscriber |
| Last Line Activity Date | The date of the previous line activity in the claim |
| Last Activity | Describes the previous action that was done on the claim |
| DOB | Date of Birth of the patient |
| DOS | Date of Service provided in the claim |
| Amount | Billed Amount in the claim |
| Previous Claim# | Claim# of the preceding claim that was sent for the same encounter |
| Claim status |
Internal: status of the claim within the practice Clearinghouse: status of the claim at the clearinghouse Payer: status at the payer end |
| Clearinghouse Response | Response from the clearinghouse regarding the claim |
| Payer Response | Response from the payer regarding the claim: Max size is 4000 characters. |
| Encounter Claim Activity | A log of previous claims that were sent on the same encounter |
| Worked | Indicates the claim has been worked on. |
Table 1