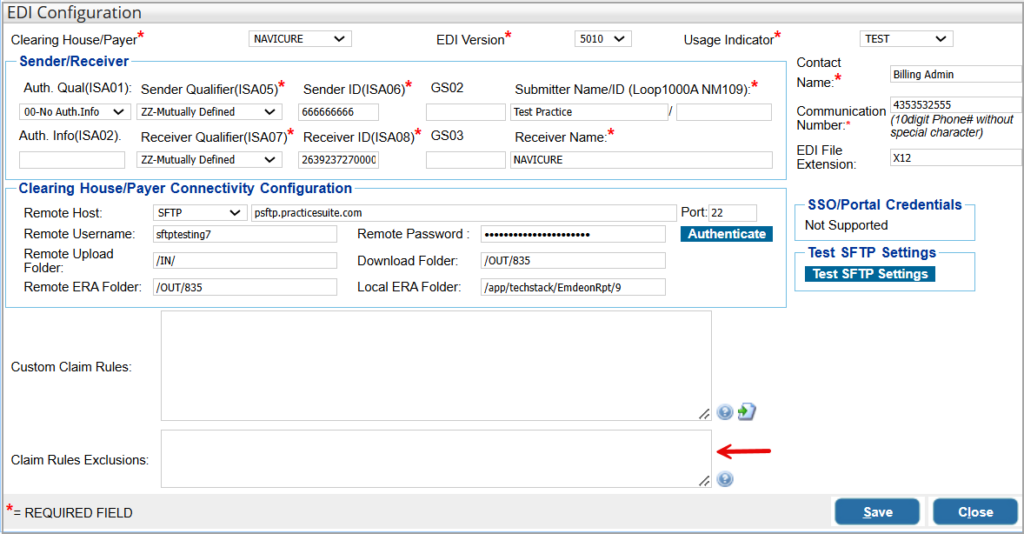
Currently running Custom Claim Rules in PracticeSuite are discussed below. Rules are clearinghouse specific. They can be viewed at EDI configuration page under Advanced Setup->Billing Options->Batch Grouping Rule->EMC Receiver ->Configure.
Custom Rules for Professional Claims
| # | Title | Description | Rule |
| 1. | To make Billing Provider Solo | [2010AA-NM1][Box33] | <PAYERID>:SOLO:PROVIDERNPI (NPI populated from provider Master) <PAYERID>:SOLO:<NPI> <PAYERID>:SOLO:<NPI>:<LAST NAME>:<FIRST NAME> <PAYERID>:SOLO:NONPI (The NPI will be blank) |
| 2. | To override Billing Provider Group | [2010AA-NM1][Box33] | <PAYERID>:GROUP:<NPI>:<GROUP NAME> <PAYERID>:GROUP:NONPI |
| 2a | To override Billing Provider Group without affecting NPI. | NPI will be populated from the LE/Practice Setup | <PAYERID>:GROUP::<GROUP NAME> |
| 3. | To set SSN instead of Tax ID | [2010AA REF02][Box 33b Other ID#] | <PAYERID>:SSN:<SSN> |
| 4. | To override the Tax ID | [2010AA REF02][Box 33b OtherID#] | <PAYERID>:TAXID:<TAXID> |
| 5. | To set taxonomy specialty ID in Billing Provider | [2000A PRV03][Box 31] | <PAYERID>:TAXONOMY:<TAXONOMY CODE> |
| 6. | To hide taxonomy specialty ID from Billing Provider | [2000A PRV03][Box 31 and 24J] | <PAYERID>:TAXONOMY:<FALSE>() |
| 7. | To put billing provider secondary ID | [2010AA REF02][Box 33b Other ID#] | <PAYERID>:SECONDARYID:<QUALIIER>:<SECONDARY ID> |
| 8. | To hide billing provider secondary ID | [2010AA PRV][Box 33b Other ID#] | <PAYERID>:SECONDARYID:FALSE |
| 9. | To include or exclude rendering provider always irrespective of any rules | [2310B][Box 31] | <PAYERID>:RENDERING:<TRUE/FALSE> |
| 10. | To include or exclude line level rendering provider | Populate/Suppress line level rendering Loop2420A in claim. To set this rule for more than one payer ID, separate them by | symbol. | <PAYERID>:24JRENDERING:<TRUE/FALSE> |
| 11. | To populate billing (33A) info in Rendering provider | [2310B][Box 31 and 24J] | <PAYERID>:RENDERING:SAMEASBILLING |
| 12. | To populate supervising provider | The rule if added with the TRUE flag will force populate the supervising provider name and NPI in the claims for the payer id. Use the FALSE flag to prevent the provider’s info from populating in the claim. | <PayerID>:SUPERVISING:<TRUE/FALSE> |
| 13. | To populate Supervising provider in Rendering provider | [2310B][Box 31 or 24J] | <PAYERID>:RENDERING:SAMEASSUPERVISING |
| 14. | To populate a specific Rendering provider in ([2310B][Box 31 or 24J]) | ([2310B][Box 31 or 24J]) | <PAYERID>:RENDERING:[<NPI>:<LAST NAME>:<FIRST NAME>] |
| 15. | To include or exclude Service location | To include or exclude Service location for payers specified in the rule | <PAYERID>:SL:<TRUE/FALSE> |
| 16. | To override Provider Accept Assignment Code | <PAYERID>:ACCEPTASSIGNMENT:<TRUE/FALSE> | |
| 17. | To include or exclude Ordering Provider Address | <PAYERID>:ORDERINGADDRESS:<TRUE/FALSE> | |
| 18. | To Exclude Pay-To-Provider | <PAYERID>:PAYTOPROVIDER:<TRUE/FALSE> | |
| 19. | For property and casualty claims, populate Member# in patient level | 2010CA REF (Y4) | <PAYERID>:WCCLAIMNUM:<TRUE/FALSE> |
| 20. | Populate the Rendering Provider in the Referring Provider field | If this rule is enabled, for the payer ids that are entered, the system will populate the rendering provider in the referring provider field. | PAYERID:REFERRING:SAMEASRENDERING |
| 21. | Populate the rendering provider PRV taxonomy code as the Billing Provider taxonomy code | This rule will populate the rendering provider PRV taxonomy code (Box 24J) as the Billing Provider taxonomy code (Box 33). | PAYERID:TAXONOMY:RENDERINGTAXONOMY |
| 22. | Populate Line Level REF IDs | If line-level REF ID needs to be populated in electronic claims, users can enter the ID # and qualifier in the Line Notes screen in Charge Master. To view all permitted reference IDs and descriptions, click here. | REF:<Qualifier>:<ID> |
| 23. | Post Patient Payments Prior to Claim Generation | When the patient payment amount has to be received by the payer and included in the claim The rule (with the flag as “TRUE“) has to be set for populating the payment amount in the electronic file. When enabled the payment info is populated in Loop 2300 with qualifier F5 | <PAYERID>:INCLUDEPATIENTPAYMENT:<TRUE/FALSE> |
| 24. | Override Place of Service | This rule is for stopping the place of service (PoS) code(s) from populating in the electronic claim for the payer ids added in the rule. This rule can be used at line level as well. | <PAYERID>:POS:<POSCODE> |
| 25. | Override Service Location for specific or all payers | Specific: <PAYERID>:SL:<NPI>:<LOCATIONNAME>:<Address>:<City>:<State>:<ZIP> All payers: <ALL>:SL:<NPI>:<LOCATIONNAME>:<Address>:<City>:<State>:<ZIP> | |
| 25a. | To blank NPI while overriding service location for specific or all payers | Specific payer: <PAYERID>:SL::<LOCATIONNAME>:<Address>:<City>:<State>:<ZIP> All Payers: <ALL>:SL::<LOCATIONNAME>:<Address>:<City>:<State>:<ZIP> | |
| 26. | Override Rendering Provider taxonomy code | This rule is for stopping the rendering provider’s taxonomy code (24J or 2310B>PRV segment) from populating in the claim for specific payers that are added in the rule | <PAYERID>:TAXONOMYRENDERING:<taxonomy id> |
| 27. | Set sender and receiver info in the EDI Header | The rule will set sender ID, Receiver ID, Receiver name in the EDI header. If <FORDOWNLOAD>is included, the info will be set only on download, else setup will be done on send and download. (Currently, this rule is not payer specific and works for payerID=ALL) | <PAYERID>:HEADER:<SENDERID>:<SENDERNAME>:<RECEIVERID>:<RECEIVERNAME><FORDOWNLOAD> |
| 28. | To replace claim number with MR# | This rule replaces the claim# in the EDI file with MR#. If <FORDOWNLOAD>is included, the rule will be applied only on download, else this rule is asserted on send and download. | <PAYERID>:CLAIMNUM:SAMEASMR:<FORDOWNLOAD> |
| 29. | To suppress/hide procedure description on the claim | <Payer_id>:CPTDESC:FALSE | |
| 30. | To populate Service location in Billing provider information | ALL:BILLING:SAMEASSL | |
| 31. | To populate the date of a similar illness as the last seen date | This rule copies ‘First date of a similar illness’ as the last seen date. | <PAYERID>: LASTSEENDATE:SIMILARILLNESSDATE |
Custom Rules Related to Institutional Claims
| # | Title | Description | Rule |
| 1. | To set taxonomy specialty ID in Billing Provider | For specific payers that are added in the rule, taxonomy specialty ID can be set in Billing provider | <PAYERID>:TAXONOMYINST:<TAXONOMY CODE> |
| 2. | To include POA (Present On Admission) Indicator | This rule is used to add POA for specific payers | <PAYERID>:POA:<TRUE/FALSE> |
| 3. | To include or exclude Service location | This rule is used to include or exclude POA for specific payers. Include- TRUE Exclude-FALSE | <PAYERID>:SL:<TRUE/FALSE> |
| 4. | To put Attending provider secondary ID | This rule sets attending provider secondary ID for specific payers | <PAYERID>:ATTENDINGID:<QUALIIER>:<SECONDARY ID> |
| 5. | To populate billing info in Attending provider |
This rule overrides attending provider info with billing provider |
<PAYERID>:ATTENDINGINST:SAMEASBILLING |
| 6. | To put service location (facility) secondary ID | This rule sets service location secondary ID for specific payers | <PAYERID>:FACILITYID:<QUALIIER>:<SECONDARY ID> |
| 7. | To populate service location in Billing Provider Address | Set this rule to TRUE if service locations is to be put in billing provider address | <PAYERID>:PUTLOCATIONADDRESSINBILLING:<TRUE/FALSE> |
| 8. | Populate Rendering Provider (Qualifier 82) in Institutional (UB04) claims | The rule when enabled will force populate the provider selected in the “Other Provider” field (FL 78) in the UB04 Charge Entry screen as the Rendering Provider (2310) | ALL:RENDERINGINST:SAMEASOTHERINST |
| 9. | Suppress Attending provider | Useful when switching the claim type from Institutional to Professional between primary and secondary. | <PAYERID>:ATTENDINGINST:FALSE |
Custom Eligibility Rules
| # | Title | Description | Rule |
| 1. | Eligibility Checks- Solo Provider | This rule if entered will force the eligibility request for a payer to be submitted using the individual Provider’s name and NPI overriding the selection in the Eligibility setup screen. | EA:<PAYERID>:SOLO:<NPI>:<LAST NAME>:<FIRST NAME> |
| 2. | Eligibility Checks- Group Provider | This rule will submit the eligibility requests for the payer using the group’s name and NPI overriding the selection in the Eligibility setup screen. | EA:<PAYERID>:GROUP:<NPI>:<GROUPNAME> |
| 3. | Annual Wellness Info through Ability CH | For clients that are on Ability clearinghouse, the system can return the annual wellness visit info in the eligibility response. The payer and procedure codes that the AWV should be returned must be indicated in the rule. | EA:<Payer ID>:CPT:<if multiple procedure codes must be added, separate them with a comma> |
| 4. | Eligibility Rule for Sending PIN | This rule is for including the PIN (Prior Identifier Number) when sending eligibility requests. | EA:<PAYERID>:REFID:<QUALIFIER>:<VALUE> Accepted Qualifiers: 0B,1C,1D,IJ,4A,CT,EL,EO,HPI,JD,N5,N7,Q4,SY,TJ |
EDI Claim Rule Exclusions
If the practice wants to exclude any specific payer from any rule, they can utilize the ‘Claim Rule Exclusions’ field to indicate the exclusion. Specify the payer and the claim rule in this field in the format given below. <payer id>:<rule> For example, to exclude the payer id ‘60054’ from the rule for copying the rendering provider as the referring provider on the charge, enter the following – 60054:REFERRING:SAMEASRENDERING into the exclusions box.