This article describes the following.
A. How to view completed clinical notes (EHR Charts) from patient portal and
B. Cures Act.
A. View or Access Completed Clinical Notes (EHR Charts) from Patient Portal
Note: Patient can view their clinical notes only if that EHR chart is saved to COMPLETE status.
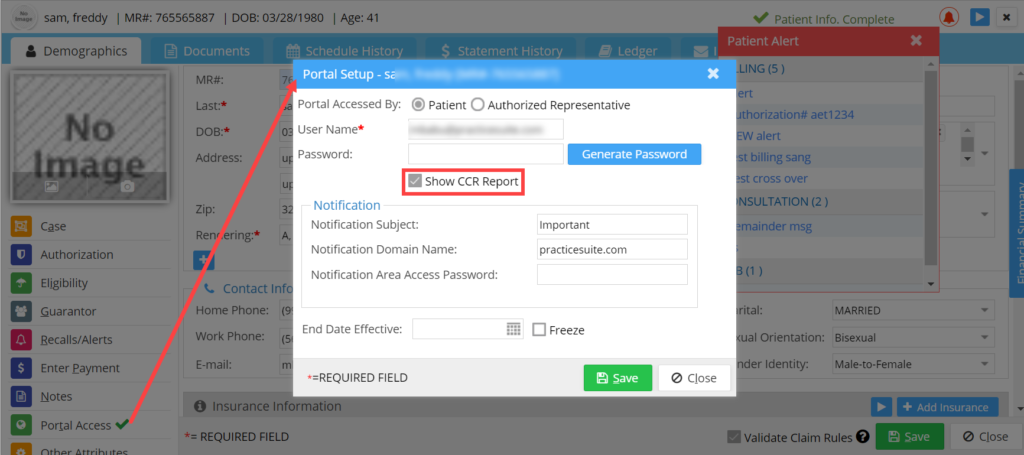
- While setting up the portal access for the patient ‘Show CCR Report‘ option should be selected in order to view their clinical notes through the portal; see Image 1.
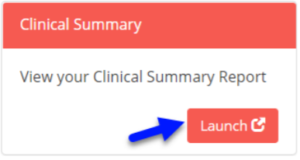
2. Login to the patient portal and click on the ‘Launch’ button under Clinical Summary section on portal screen; see Image 2.
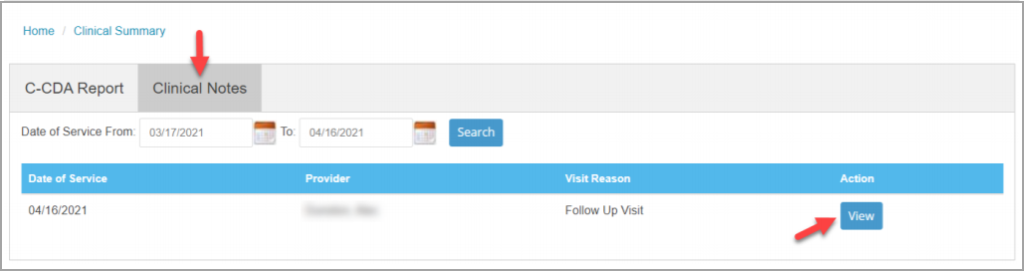
3. From the clinical summary page, select the ‘Clinical Notes’ tab to view the list of completed clinical notes of the patient; see Image 3.
a. Provide the date range and click on the Search button to view all the clinical notes in that date range. By default, system will be listing the completed clinical notes of the previous 30 days.
b. Each row in the listing displays the visit details like Date of Service, Rendering Provider from Chart, Visit Reason from appointment and a View button to access the clinical note for that visit.
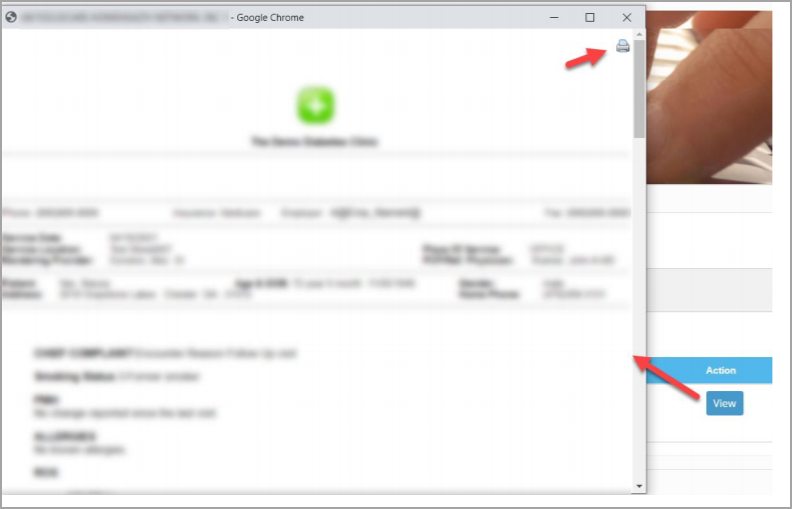
c. Clicking on the View button (highlighted in Image 3) against the visit opens a popup window having the clinical note/narration of that visit. Clients have an option to print the clinical note/narration( see highlighted part on the top right part of Image 4).
B. Cures Act
ONC’s Cures Act Final Rule supports seamless and secure access, exchange, and use of electronic health information.
From April 5, 2021, the program rule on Interoperability, Information Blocking, and ONC Health IT Certification, which implements the 21st Century Cures Act, requires that healthcare providers give patients access without charge to all the health information in their electronic medical records.
PracticeSuite is compliant with CURES Act; Our current ONC certification will cover our end users.
The eight (8) types of clinical notes that must be shared are outlined in the United States Core Data for Interoperability (USCDI), and include:
1.Consultation notes
2. Discharge summary notes
3. History & physical
4. Imaging narratives
5. Laboratory report narratives
6. Pathology report narratives
7. Procedure notes
8. Progress notes
Clinical notes to which the rules do not apply:
- Psychotherapy notes that are separated from the rest of the individual’s medical record and are recorded (in any medium) by a health care provider who is a mental health professional documenting or analyzing the contents of conversation during a private counseling session or a group, joint, or family counseling session.
To know more on Cures Act, visit