Physicians need to verify each patient’s eligibility and benefits to ensure they will receive payment for services rendered. The main objective of eligibility verification is to prevent denials and avoid delays in payment, save time on the back end, and also enhance patient satisfaction. The following are the steps in the configuration of eligibility verification.
1. Select Setup from the main menu and then choose Practice. Select the required Practice from the list of practices shown on the left for which Eligibility Verification functionality needs to be configured. Now click on ![]() button on the top right part of the screen.
button on the top right part of the screen.
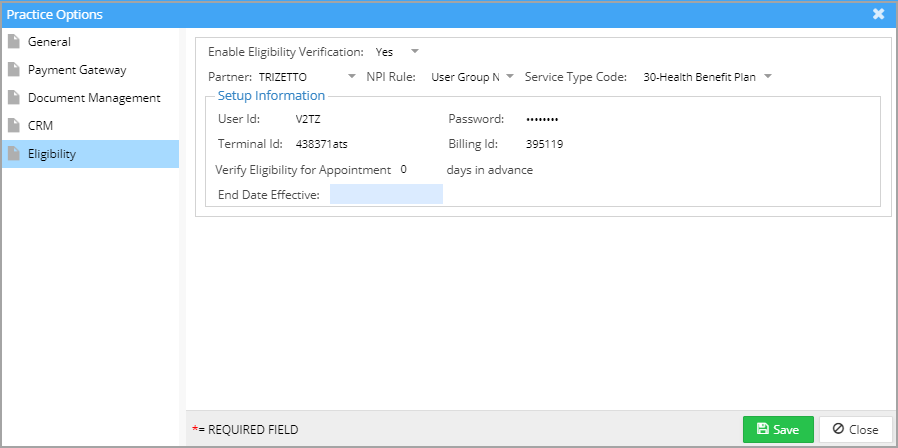
2. Click on the Eligibility tab of Practice Options and the following screen opens up.
The following are the fields in the Eligibility tab.
Enable Eligibility Verification: If the practice requires eligibility verification by a clearinghouse, set this option to YES and a drop-down appears for selecting the clearinghouse. If set to NO, the practice will not be able to do eligibility verification.
NPI Rule: Select the rule to be applied in verification.
Service Type Code: Select the service for which the eligibility is to be verified.
Set Up Information
The fields in the Set-Up Information box such as User Name, Password, Terminal ID, Billing Id, etc. are credentials provided to the practice for accessing the clearinghouse server for eligibility verification.
Verify Eligibility for Appointment: If automatic verification of eligibility is required, set the number of days prior to the appointment when the verification is to be done.
End Date effective: The date on which automatic verification of eligibility is to be stopped.