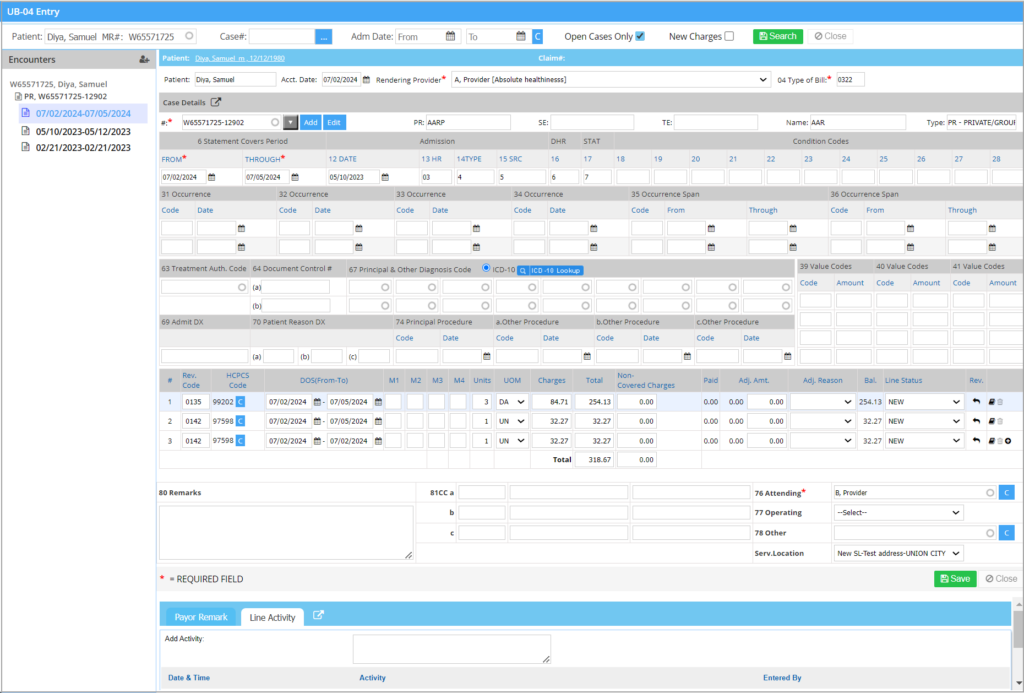
The UB04 Charge Entry
UB04 Charge Entry screen manages the entry and editing of UB04 charges. Some key points related to UB04 Charge Entry are:
1. UB04 charge entry is used for institutional claims only.
2. There is no mapping between procedure codes and diagnosis.
3. Revenue codes are mandatory, whereas procedure codes are not.
4. A print option is available on the UB04 charge entry screen (see Image 1). This feature allows users to print the UB04 claim form directly from the screen, similar to the professional claim’s charge entry screen feature.
A Sample UB04 Charge Entry Screen
All institutional cases and corresponding encounters are displayed on the left. To add a new encounter, click on ![]() button in the Encounters pane. To edit an encounter, click on encounter on the left. Table 1 describes the important fields in the UB04 charge entry screen. Box numbers in the UB04 charge entry form are given in brackets wherever applicable.
button in the Encounters pane. To edit an encounter, click on encounter on the left. Table 1 describes the important fields in the UB04 charge entry screen. Box numbers in the UB04 charge entry form are given in brackets wherever applicable.
Note:
1. New lines cannot be added to existing charges with a closed accounting period.
2. If the acct. date of the charge falls in a closed accounting period, the acct. date will no longer be modifiable.
3. The Payer Remark and line Activity tab in the UB04 screen and Charge Master perform similarly. Line Activity showing ERA payment posting will have the payment# link to the ERA.