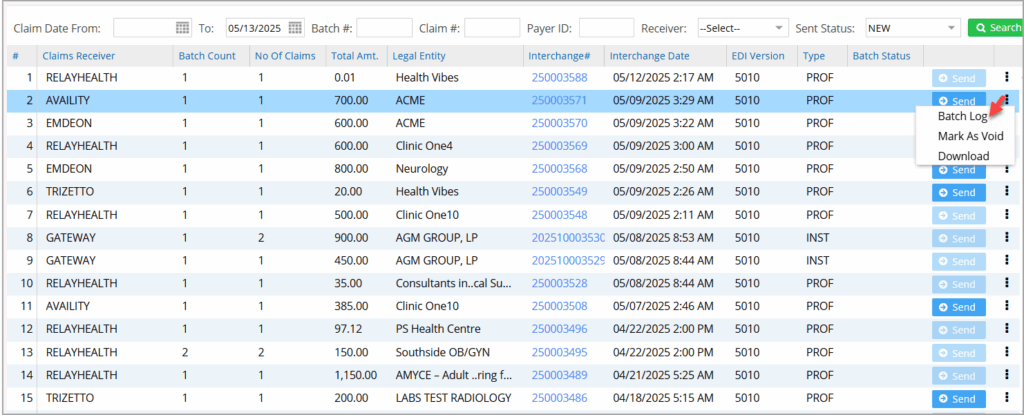
The Claims Dashboard provides detailed information on every claim generated in the system. The dashboard has a pie chart representation to get a quick view of the number of claims in the different statuses. Image 1 is a sample screenshot of the dashboard.
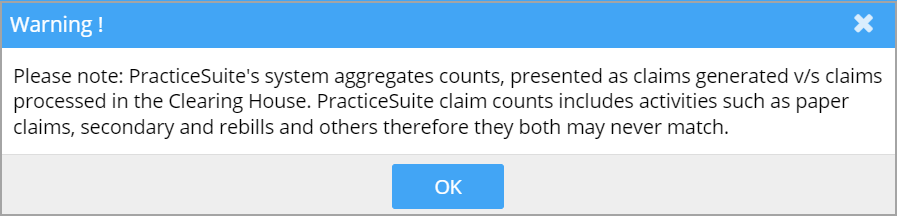
Note: The Info icon (arrow-marked in the above image) will display the following message when clicked.
The left pane shows the different buckets (that represent the various statuses) and the number of claims in the bucket as of the claim date selected at the top of the dashboard. The default date range is 30 days before the current day.
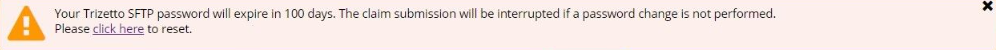
SFTP Password Reset for Trizetto: PracticeSuite will begin to warn users of Trizetto SFTP password expiration 20 days before the expiration date. The warning pop-up will appear on the Claims Workbench screen, and there will also be a link in the pop-up to reset their user password.
Buckets: The different buckets in the dashboard are the following: Out of these, the response buckets are Accepted, Clearinghouse Rejects, Payer Rejects, and Pending Responses. These buckets have search filters for claim date, patient, and insurance.
Buckets in the Claims Dashboard
1. Ready To Submit
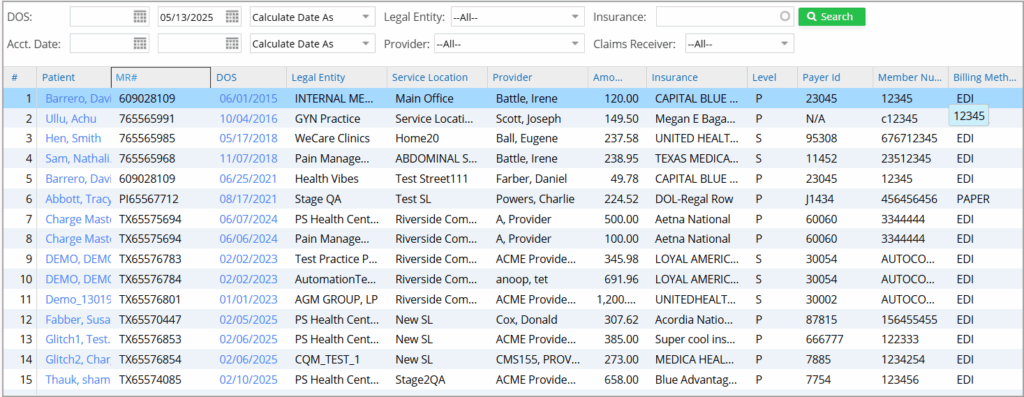
Claims under this bucket are not yet submitted but are ready. ‘Ready’ in this context means that the charges are entered and verified to be sent. All claims initially fall into this bucket. Refer to image 2.
2. Unsubmitted Batches & Error Batches
Claims batched and ready to be sent to clearinghouses are placed in the unsubmitted bucket.
Batches found to be error-prone fall into error batches. The system does the verification. Users can take corrective measures and batch them again to be submitted.
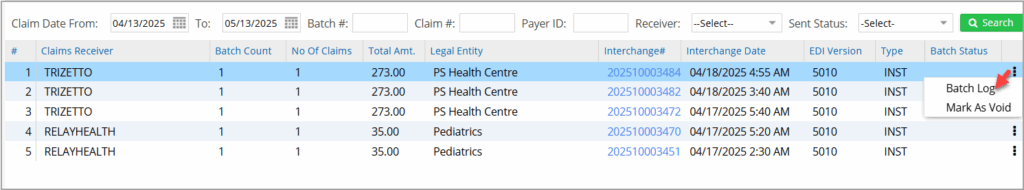
Users can void unsubmitted claim batches. The ellipsis menu provides the Mark as Void option. Users can void an entire batch to prevent it from being transmitted, maintaining accuracy in claim management. Furthermore, the Download and Batch Log options are now under the ellipsis menu to enhance navigation. Image 2 shows the unsubmitted bucket and Image 3 shows the error batch.
3. Accepted
Electronic claims for which the clearinghouse has okayed or the corresponding insurance has agreed to pay in full or partially fall into this bucket. Refer to Image 4
4. Clearing House Rejects
Electronic claims which have been rejected by the clearinghouses fall in this bucket. Click here to view a detailed discussion on typical clearinghouse rejections from Trizetto.
5. Payer Rejects
Claims rejected by the payer fall into this bucket. Rejections occur due to invalid data or missing information.
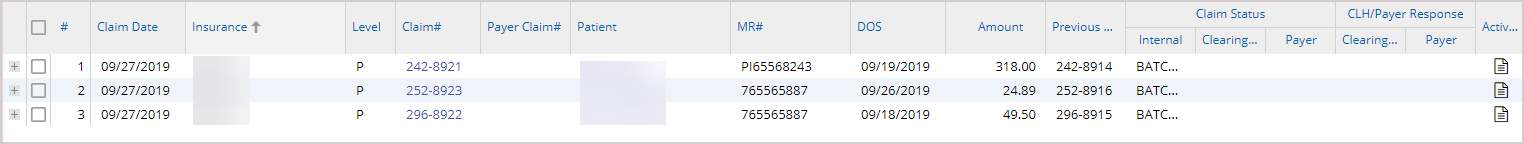
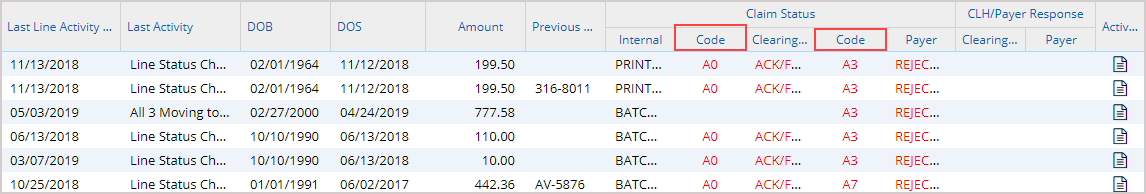
Note: For claims rejected by either the clearinghouse or payer, the rejection code is displayed in the rejection buckets and on the Claims History tab. Image 5 shows a part of the Claims History tab. The highlighted fields in the image are the clearinghouse rejection code and the payer rejection code.
6. Pending Responses
The payer or the clearinghouse responds within five days of claim submission. Claims for which no response has yet been received even after five days, fall in this bucket.
7. Downloaded
Electronic claims downloaded into the system can be viewed here.
8. New paper
Ready paper Claims (charges entered and verified) fall into this category.
9. Printed
This bucket contains paper claims already printed.
10. Hold
Lines in Hold status will appear under the Hold Lines bucket. Lines in the HOLD_Type sub status will be under separate buckets under the Hold category. Claims in these buckets will be excluded from batching and claim generation.
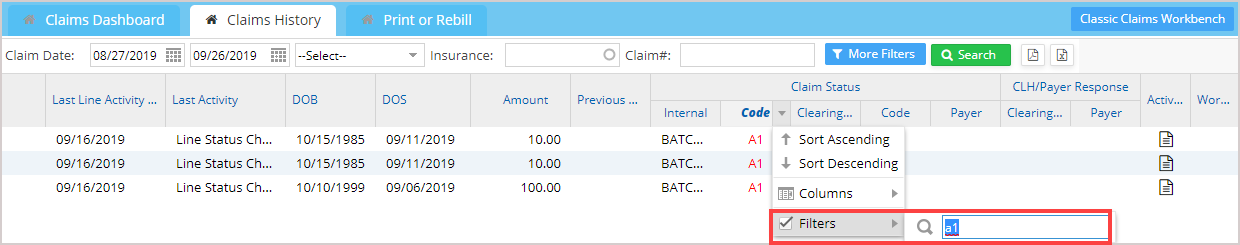
Further Filtering of Columns in Claims Listing
Every tab in the claims workbench has filtering at the column level, wherein claim listings can be further filtered by payer, clearinghouse, patient, claims status code, and others. All the fields are available for filtering except date fields, amounts, and number fields. Filter applied for status code with value ‘a1’ is illustrated in Image 6.